
Annemiek van Vleuten was badly injury by an over the handle bars crash in the 2016 Olympics.
After a blow to the head, the survivor, her family, friends, co-workers all expect the injured person to “be okay.” After initial weeks of recovery it seems like that’s the case. However, if you can get this injured person to stop normalizing the odd things she’s experiencing and be totally honest, you will hear that survivor of a brain injury still experiences significant cognitive changes weeks and months after the incident. This means “it’snot okay.” She still is suffering, still struggling, still recovering and not back to “normal. In my 31 years of helping injured people I know this is what happens. I see it with all my patients. Most medical specialists who help survivors of concussion/Traumatic Brain Injuries will tell you there remains a continuing condition which will never “be okay.” In an in depth study published in the Journal of Neurotrauma, “Traumatic brain injury: a disease process, not an event” two neuroscientists report findings of what I have known for more than thirty years: Brain trauma does not go away. They report: “Traumatic brain injury (TBI) is seen by the insurance

This helmet saved Ben Hobb’s life in 2015, but didn’t stop him from having a brain injury.
industry and many health care providers as an ‘event.’ Once treated and provided with a brief period of rehabilitation, the perception exists that patients with a TBI require little further treatment and face no lasting effects on the central nervous system or other organ systems. In fact, TBI is a chronic disease process, one that fits the World Health Organization definition as having one or more of the following characteristics: it is permanent, caused by non-reversible pathological alterations, requires special training of the patient for rehabilitation, and/or may require a long period of observation, supervision, or care. TBI increases long-term mortality and reduces life expectancy. It is associated with increased incidences of seizures, sleep disorders, neurodegenerative diseases, neuroendocrine dysregulation, and psychiatric diseases, as well as non-neurological disorders such as sexual dysfunction, bladder and bowel incontinence, and systemic metabolic dysregulation that may arise and/or persist for months to years post-injury.” The two researchers want the medical community to make “classification of TBI as the beginning of an ongoing, perhaps lifelong process, that impacts multiple organ systems and may be disease causative and accelerative. ….not to discourage patients with TBI or their families and caregivers, but rather to emphasize that TBI should be managed as a chronic disease and defined as such by health care and insurance providers. Furthermore, if the chronic nature of TBI is recognized by government and private funding agencies, research can be directed at discovering therapies processes months or even years that may interrupt the disease after the initiating event.”
Head trauma with subsequent injury to the underlying brain tissue with or without intracranial bleeding can be extensive and obvious clinically but can also be occult and difficult to diagnose even with the best of clinical Neurological and Psychological testing. in many cases, mild or subtle cases of TBI evolve into chronic traumatic encephalopathy (CTE). The Center for Disease Control in Atlanta Georgia states: “Chronic Traumatic Encephalopathy is a progressive neurodegenerative disease (tauopathy) caused by total brain trauma, and is not limited to athletes who have reported concussions. The typical signs and symptoms of CTE include a decline of recent memory and executive function, mood and behavioral disturbances (especially depression, impulsivity, aggressiveness, anger, irritability, suicidal behavior and eventual progression to dementia). The initial signs and symptoms do not typically manifest until decades after trauma received (ages 40-50). someone in their teens or 20s who suffers a severe brain trauma would not show noticeable signs of it for decades. Fortunately, new software called Neuroquant is available to the injured person who notices ssymptoms of CTE. Sometimes, it gets worse: a small subset of individuals with CTE develops Chronic Traumatic Encephalomyopathy (CTEM). This isa progressive motor neuron disease characterized by profound weakness, atrophy, spasticity and fasciculation similar to amyotrophic lateral sclerosis (ALS). CTE is responsible for significant interference with the activities of daily living. The CT scan that a Hospital emergency department orders is useless for these types of traumatic brain injury. Even the usual MRI ordered by a concerned family physician will not likely show damage to the cells in case of a traumatic brain injury. A family physician usually spacedoes not know which is the proper MRI test to order. There are several different kinds. While even the best quality Neuro-anatomical structural imaging may still not uncover responsible brain pathology, newer functional brain MRI techniques on the 3.0 Tesla scanner promise to be more successful.
Of particular utility are the functional BOLD 3.0 Tesla MRI sequences (VEN_BOLD SWI) which are as much as 4 -6 times more sensitive than gradient echo (GRE) T2* 1.5 Tesla images and twice as sensitive as 3.0 Tesla GRE sequences at detecting occult micro-hemorrhages in the brain which might be associated with axonal shear injury. Overall, the SWI sequences are roughly 6 times more likely than routine, non-susceptibility 1.5 Tesla imaging to detect old blood deposits in brain. Other MRI tests for traumatic brain injury include DTI and, the latest, Neuroquant.
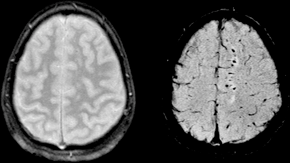
By SBarnes – Karen Tong, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=5874994
Take a look at the white spots in this MRI. Those spots are where the brain has suffered “Diffuse Axonal Injury” or DAI. These spots can be big or small. They are all pictures of the death of brain cells.
This is not what the insurance industry and the impatient family practice doctor will recognize. According to neurotrauma researchers the slow death of the white
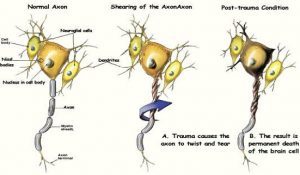 and the injury to adjacent brain cell axons after trauma is like a “suicide/murder.” One medical illustration company has a video explaining this. ¹
and the injury to adjacent brain cell axons after trauma is like a “suicide/murder.” One medical illustration company has a video explaining this. ¹
It seems like you keep struggling and you’re not getting better and your doctor doesn’t understand or care or your loved one and friends can’t help. My clients have been where you are. I helped them recover too.
I understand.
I can help you
I received a bachelor of science degree in Psychology with a minor in biology from Florida State University. The brain is our most important human organ. It can be badly damaged with what the emergency department or walk-in clinic calls a “concussion.” It’s not an injury to be taken lightly and it needs to be understood. It doesn’t go away. You recover, but you have a permanent injury which has to be properly evaluated and understood. The CDC has an entire page on this one injury alone because it is so important to us and our brains.
I understand.
If you are injured and searching the web for an attorney, stop clicking.
stop clicking.
I am a full-service personalized, personal injury lawyer with a statewide practice in all 67 counties. I have 31 years of experience to put to work for you. Call so I can answer your questions: 1-800 – 535 – 3002. Email: [email protected] Skype: ScienceCan Facebook: https://www.facebook.com/JSteeleLaw/ Twitter: @JsteeleOlmstead or @FlaBicyleLawyr Instagram: jsteeleolmstead.
